For women, breast cancer is a dreaded and devastating disease. Over a lifetime, one in eight American women are affected by breast cancer. It is the most commonly diagnosed cancer and the second leading cause of cancer death in women. Although currently there is no way to prevent breast cancer, early detection is a woman's best hope for effective treatment and better survival rates.
Currently, breast cancer can be detected through a breast examination by a physician or by the woman herself; or conventional x-ray mammogram, which can find a tumor that is too small to be discovered by breast self-exam.
The use of technology to produce a picture of the breast is termed "imaging." Imaging is used several ways, among them:
Screening: Cancers found by screening mammography have a greater chance for cure and may be treated without mastectomy.
Diagnosis: Image-guided needle biopsies can replace many surgical biopsies, reduce cost, and eliminate scarring.
When to have a mammogram
The American Cancer Society recommends the following:
Women age 40 and older should have a screening mammography every year.
Between the ages of 20 and 30, women should have a clinical breast examination by a health professional every three years. After age 40, women should have a breast exam by a health professional every year.
Women age 20 or older should perform breast self-examination every month.
Mammography
Conventional mammography is the way most breast imaging is performed. It is a technique that uses x-rays to create an image of the breast tissue on film. During a mammography, a woman undresses to the waist and stands in front of the mammography equipment, where her breast is slowly pressed between a plastic plate and the film while the x-ray is taken.
This "flattening" technique generally takes a few seconds. Typically, two x-rays are taken of each breast; more may be needed to view areas of special concern.
In recent years, advances have improved the procedure and reduced the radiation dose to very low levels. Even with technical advances in x-ray mammography there are still problems distinguishing malignant from benign tumors.
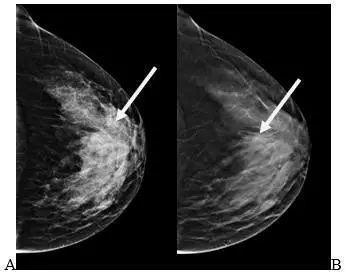
Three of four lesions that it detects are benign, resulting in unnecessary biopsies. Mammography misses about 15 percent of cancers. Many of the missed cancers occur in women with dense breast tissue. About 40 percent of women have dense breasts and this type of tissue can mask the presence of a tumor.
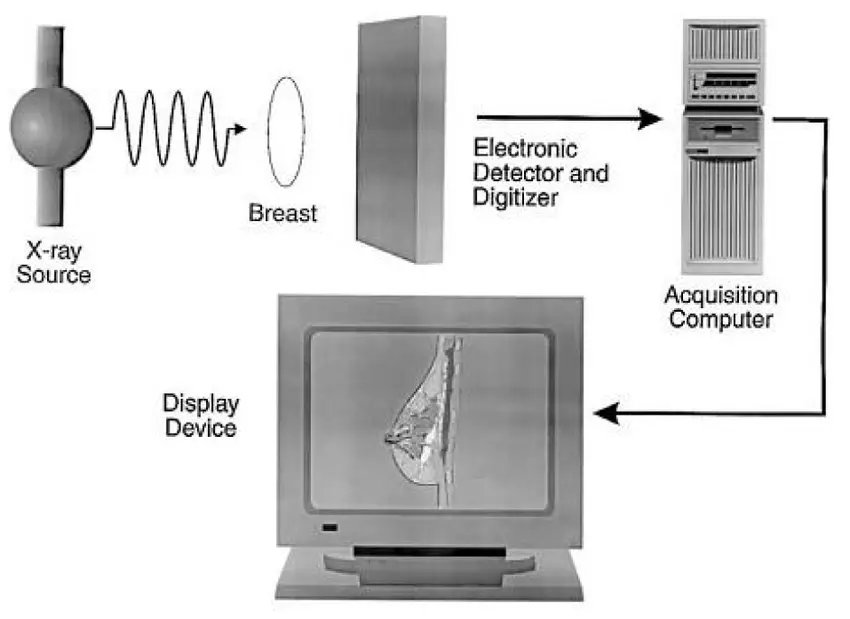
Digital mammography represents a transformative leap in the early detection and management of breast cancer, combining advanced imaging technology with digital data processing to dramatically improve diagnostic accuracy and patient outcomes. Unlike traditional film-based mammography, which captures images on X-ray film, digital mammography uses electronic detectors to convert X-rays into high-resolution digital images that can be viewed immediately on a computer screen. This allows radiologists to manipulate the images zooming in, adjusting contrast, enhancing brightness, or magnifying specific areas to detect even the smallest abnormalities, such as microcalcifications or tiny masses that may indicate early-stage cancer. This feature is particularly crucial in women with dense breast tissue, where overlapping tissue structures can obscure lesions in conventional images. The increased clarity and flexibility provided by digital systems greatly improve the sensitivity and specificity of screening, reducing false negatives and unnecessary follow-up procedures. Additionally, digital images can be stored electronically, allowing for long-term archiving, remote consultations, and integration with other diagnostic technologies such as Computer-Aided Detection (CAD) systems and Artificial Intelligence (AI) tools. These systems analyze mammograms to highlight areas of concern that may require further investigation, acting as a second set of eyes for radiologists and increasing overall diagnostic confidence.
One of the most impactful advancements stemming from digital mammography is the development of digital breast tomosynthesis, also known as 3D mammography, which captures multiple images of the breast from different angles to create a layered, three-dimensional view. This technique reduces the effect of overlapping tissue and improves the detection of invasive cancers, particularly in women with dense breasts. Furthermore, digital mammography is well-suited to image-guided interventions such as biopsies, where the precise location of a suspicious lesion must be identified and targeted with minimal invasiveness. This integration with interventional radiology helps ensure timely diagnosis and effective treatment planning.
From a public health perspective, digital mammography is a critical component of organized breast cancer screening programs worldwide. It enables faster screening workflows, easier data sharing, and population-level health monitoring through electronic health records. In countries like India, where breast cancer has become the most commonly diagnosed cancer among women and late detection remains a major challenge, the adoption of digital mammography offers an opportunity to expand access to quality screening in both urban and rural settings. Portable and mobile digital mammography units can now bring screening services to underserved communities, enhancing equity in cancer care.
For the patient, digital mammography offers several tangible benefits: the procedure is generally quicker and more comfortable, images are available almost instantly, repeat exams are less common, and radiation exposure is lower compared to traditional methods. These advantages contribute not only to improved clinical outcomes but also to greater patient satisfaction and compliance with regular screenings. In sum, digital mammography is a cornerstone of modern breast cancer diagnostics a perfect example of how imaging innovation, data science, and biotechnological progress can converge to deliver earlier detection, more accurate diagnosis, and ultimately, better chances of survival for millions of women around the world.